Think you’ve got resistance figured out? Let’s test that. 10 questions, one theme: antimicrobial resistance mechanisms. Try not to overthink it – but also, maybe do.
Again, this is a soft launch and not all of the features have been fine-tuned. The answers are directly under each question, so try not to cheat. The universe is watching.
D. Serratia lost its VIP AmpC status – Recent studies indicate that clinically significant AmpC production occurs in less than 5% of Serratia, Providencia, and Morganella. ID folks now favor the HECK Yes lineup (Hafnia, Enterobacter, Citrobacter, Klebsiella, Yersinia) for true inducible AmpC troublemakers.
True. Bacteria can’t have it all. The see-saw effect describes how when they bulk up their defenses against daptomycin, they often drop their guard against humble beta-lactams. This phenomenon has been observed in various studies, including those focused on Staphylococcus aureus and Enterococcus faecium.
B. Durlobactam isn’t the star of the show — but it keeps the lights on. By inhibiting class D beta-lactamases like OXA-23, it allows sulbactam to actually do its job. Porin channels and ribosomes can sit this one out.
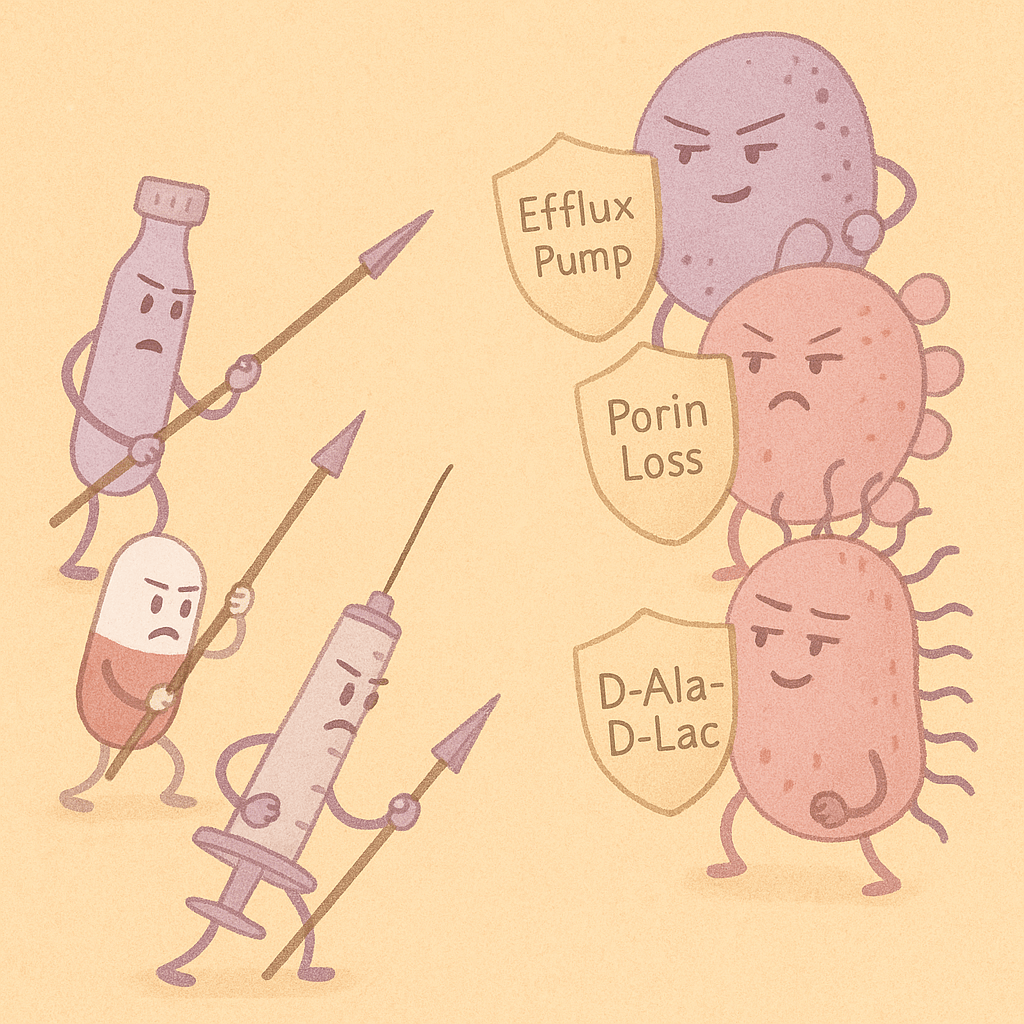
C. vanA isn’t subtle — it swaps out D-Ala-D-Ala for D-Ala-D-Lac in the peptidoglycan precursor, reducing vancomycin’s binding by ~1,000-fold. That’s not a typo. This is biochemical ghosting at its finest.
B. Pseudomonas doesn’t just pump iron — it pumps out your fluoroquinolones too. The MexAB-OprM efflux system is a major player in its multi-drug resistance. If you’re wondering why your levofloxacin didn’t work, it may have just been kicked out the back door.
A. Proteus doesn’t do bladder-only drama — its alkaline urine and intrinsic resistance to nitrofurantoin make it a bad match for this go-to UTI agent. If you see it, don’t reach for your Macrobid.
B, C, D. Quinolone resistance is usually a team effort: mutation at the target (DNA gyrase or topo IV), combined with reduced drug entry and increased efflux. Enzymatic breakdown? Not this time — that trick’s more for the beta-lactam crowd.
C. mecA encodes PBP2a, a penicillin-binding protein that has poor affinity for most beta-lactams — with notable exceptions like ceftaroline, which was designed to get around that.
B. katG encodes catalase-peroxidase, the enzyme that activates isoniazid. Knock it out, and the drug can’t do its job. Resistance via katG mutation is one of the classic high-yield facts for a reason — it sticks (unlike your patient’s adherence to DOT).
Leave a comment